About the Intervention
The intervention involves a narrative interview and safety plan followed by solution-focused follow-up sessions.
The narrative interview involves the person being asked to tell their story leading up to the crisis to the practitioner. They will then create an enhanced safety plan with the practitioner, following a collaborative planning process. Within 72 hours of leaving the Emergency Department, the person will receive a check-in phone call from the practitioner.
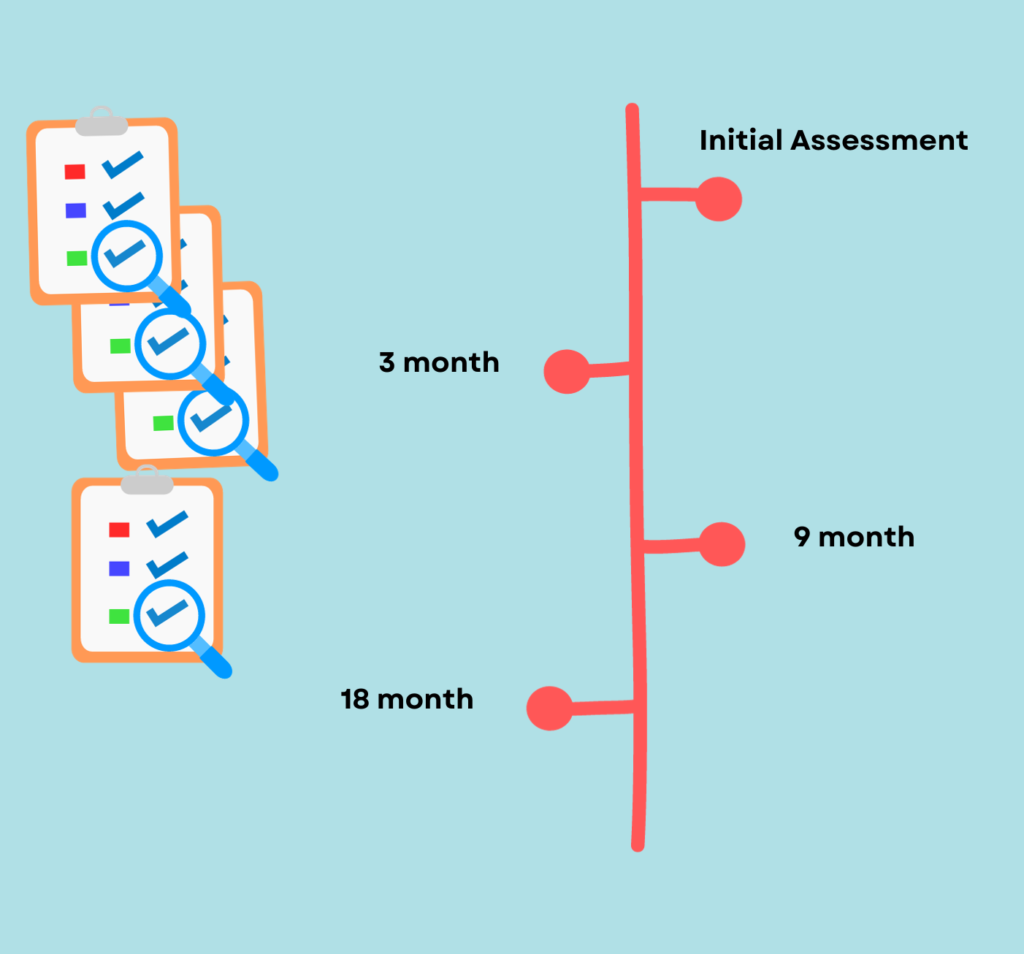
They will be offered face-to-face; telephone; and/or online video-conference meetings over a two-month period with the same practitioner to discuss the patient’s main concerns and, using a solution-focused approach, collaboratively formulate solutions to address these concerns. At three, six and nine months, the person will receive personalised letters to remind them of the safety plan and support networks.
Initial meeting in the ED
Meeting in the Emergency Department (ED)
One week follow up
Four week follow up
Eight week follow up
Letters at 3, 6 and 9 months.
We piloted the intervention in four Emergency Departments with people who had presented with self-harm. We sought feedback to learn from the experiences of practitioners and patients, to help us to refine the approach.